In the world of elite sports and high-performance training, the pursuit of physiological advantages is ceaseless. Athletes and coaches often focus on major hormonal levers to maximize strength, recovery, and endurance. Among these, testosterone is perhaps the most discussed, utilized, and manipulated hormone. While its role in muscle hypertrophy and neural drive is widely recognized, testosterone also plays a critical, often underappreciated role in hematology—specifically, the production of red blood cells.
However, physiology is rarely a simple linear equation. The body’s intricate systems rely on dependent variables. Emerging understanding of iron metabolism reveals a crucial caveat in the hormonal pursuit of performance: testosterone’s ability to enhance oxygen transport is fundamentally limited by the body's iron status. Without adequate iron, the hormonal signal to build better blood is rendered ineffective.
The Oxygen Imperative in Athletics
For endurance athletes, team sport players, and mixed martial artists alike, oxygen delivery to working muscles is the cornerstone of performance. This is governed by the blood's oxygen-carrying capacity, primarily dictated by the total mass of hemoglobin contained within red blood cells via a process called erythropoiesis.
Historically, methods to increase red blood cell count—from high-altitude training to illicit blood doping with erythropoietin (EPO)—have been sought to gain a competitive edge. Testosterone is a powerful, naturally occurring accelerator of this very process.
The Hormonal Mechanism: Hepcidin and Ferroportin
To understand how testosterone influences blood production, one must understand the body's iron regulatory system. Iron is essential for creating hemoglobin, but it is also highly reactive and toxic if left unbound in the bloodstream. Therefore, its movement is tightly controlled.
The central regulator of iron in the human body is a liver-derived peptide hormone called hepcidin. Hepcidin acts as the physiological "brake" on iron absorption and mobilization. When hepcidin levels are high, iron is locked within storage cells (macrophages and hepatocytes) and absorption from the gut is blocked.
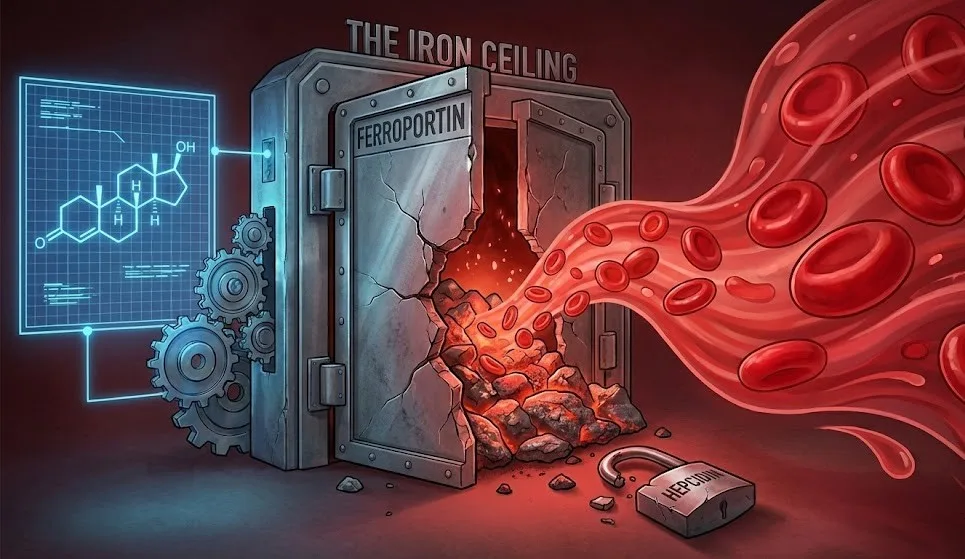
The primary "gate" that lets iron out of storage and into circulation is a protein transporter called ferroportin. Hepcidin works by binding to ferroportin and degrading it, effectively closing the gate.
This is where testosterone enters the equation. Research indicates that testosterone—whether endogenously produced or exogenously introduced—suppresses the expression of hepcidin mRNA. By lowering hepcidin levels, testosterone removes the "brake." Consequently, the activity of ferroportin increases. The gates open, allowing stored iron to flood into the bloodstream, ready to be utilized for erythropoiesis.
The Critical Bottleneck: Serum Iron Availability
While testosterone effectively signals the body to mobilize iron and initiate red blood cell production, this signaling pathway contains a critical fail-safe. The entire process is predicated on the actual presence of the raw material: iron.
The increased activity of ferroportin is only functional if there is sufficient serum iron available to be transported. If an athlete is iron-deficient, opening the "ferroportin gates" achieves nothing because there is nothing behind the gate to release.
This leads to a vital physiological reality: in the presence of iron deficiency, erythropoiesis (the production of new red blood cells stimulated by EPO) stalls. The hormonal signal from testosterone may be screaming for more oxygen-carrying capacity, but without the requisite iron atoms to form the hemoglobin core, the bone marrow cannot comply. The machinery exists, the signal is present, but the fuel is missing.
Implications for the Athlete
This biological mechanism has profound implications for athletes, particularly those engaged in heavy training loads.
1. The Danger of Assumed Gains: Athletes using testosterone replacement therapy (TRT) or performance-enhancing substances often assume a guaranteed increase in endurance and recovery. However, if their baseline iron stores (ferritin) are low, they will hit an "iron ceiling," failing to realize the hematological benefits of the hormone.
2. Functional Iron Deficiency in Training: Intense athletic training itself creates a challenge. High-intensity exercise induces inflammation, which naturally raises hepcidin levels (the body's attempt to sequester iron from potential pathogens during perceived stress). This athlete might have adequate iron stored in their body, but high hepcidin keeps it locked away, making it unavailable for red blood cell production. Testosterone helps counteract this exercise-induced rise in hepcidin, but only if the athlete isn't already depleted through sweat, gastrointestinal bleeding, or foot-strike hemolysis.
3. The Necessity of Comprehensive Bloodwork: Focusing solely on hormonal profiles while neglecting micronutrient status is a critical error in performance management. Monitoring serum iron, total iron-binding capacity (TIBC), and especially ferritin (storage iron) is as essential as monitoring testosterone levels.
Conclusion
The human body operates on synergy, not isolated signals. Testosterone is a potent conductor of physiological adaptation, capable of significantly boosting an athlete's oxygen-carrying capacity by modulating iron transport. Yet, a conductor cannot make music without instruments. Iron is the fundamental instrument of blood. For athletes seeking peak performance, recognizing that powerful hormonal signals are ultimately dependent on basic nutritional building blocks is essential to avoiding the iron ceiling and maximizing potential.