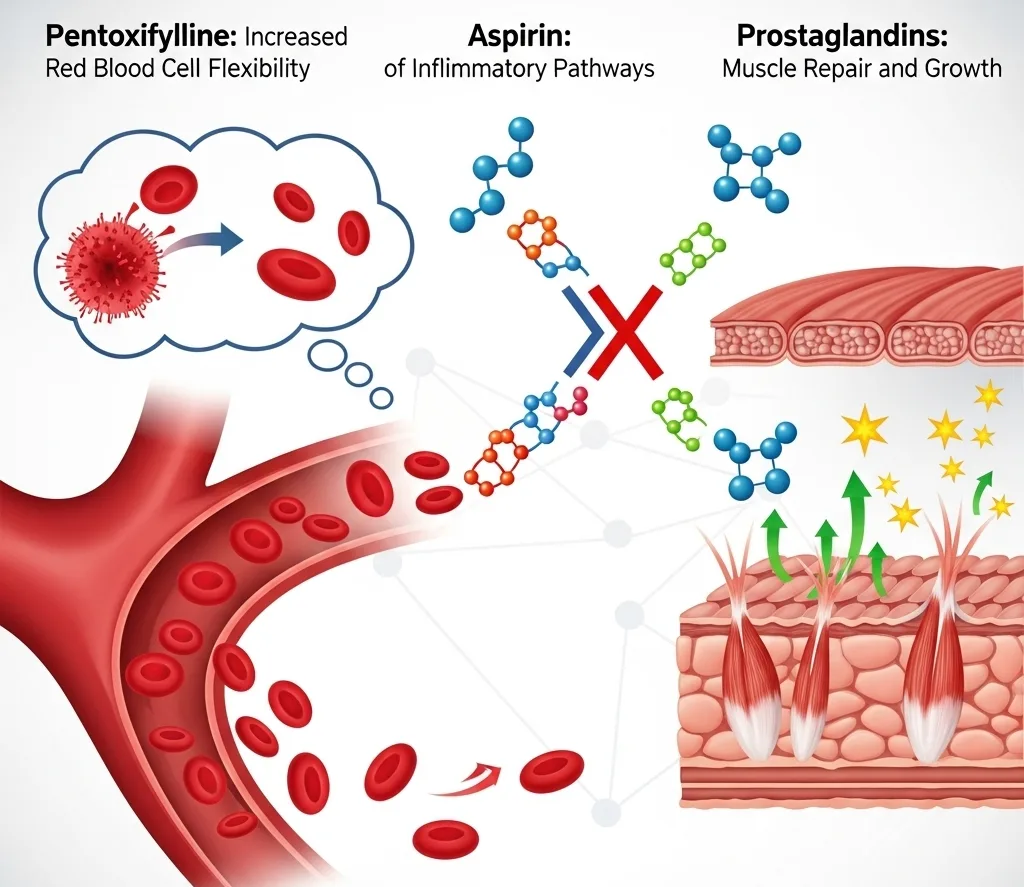
When it comes to treating blood flow issues, especially those related to peripheral artery disease (PAD), the choice of medication is not about which drug is universally "better," but rather which one is the most effective for a specific problem. Pentoxifylline stands out from treatments like aspirin and prostaglandins due to its unique mechanism of action, making it a superior choice for certain aspects of the disease.
The core difference lies in how each drug improves blood flow:
Aspirin focuses on platelets to prevent clotting.
Pentoxifylline focuses on the blood itself, improving its flow properties.
Pentoxifylline's Unique Advantage
Pentoxifylline is a xanthine derivative that is often used to treat intermittent claudication, a common symptom of PAD characterized by leg pain during exercise. It's a hemorheologic agent, meaning it improves the way blood flows. Pentoxifylline works in two key ways:
Increases Red Blood Cell Flexibility: It makes red blood cells more pliable and able to squeeze through narrow, constricted arteries. In PAD, red blood cells can become rigid, making it harder for them to navigate the already narrowed vessels.
Reduces Blood Viscosity: It thins the blood, making it less "sticky" and easier to circulate. This is especially helpful when combined with the improved red blood cell flexibility.
By addressing the blood's intrinsic properties, pentoxifylline improves microcirculation and oxygen delivery to the muscles in the legs, which can reduce pain and increase walking distance for patients with PAD.
Why Pentoxifylline May Be a Better Choice Than Aspirin
Aspirin is a nonsteroidal anti-inflammatory drug (NSAID) and, more importantly in this context, an antiplatelet agent. Its primary role is to prevent platelets from clumping together to form blood clots. It does this by inhibiting the cyclooxygenase (COX) enzyme, which is responsible for producing various prostanoids, including prostaglandins. One such prostaglandin, thromboxane A2, is a powerful promoter of platelet aggregation. By lowering the production of these clotting agents, aspirin reduces the risk of clot formation that could lead to a heart attack or stroke.
This mechanism is why aspirin is so crucial for cardiovascular risk reduction. However, it does not directly address the underlying symptoms of intermittent claudication. It does not make red blood cells more flexible or reduce blood viscosity. Therefore, for a patient whose main complaint is leg pain that limits walking, pentoxifylline directly targets the cause of the symptom, offering a benefit that aspirin does not.
In many cases, a patient with PAD may be prescribed both aspirin (for cardiovascular risk reduction) and pentoxifylline (for symptomatic relief), as they serve two completely different purposes due to their distinct mechanisms.
The Role of Prostaglandins in Muscle Buildup and Performance
While some prostaglandins (like thromboxane A2) are associated with clotting and inflammation, others play a vital and beneficial role in muscle physiology. The body produces different types of prostaglandins in response to various stimuli, and some of these are crucial for muscle repair and growth.
For athletes, especially those engaged in resistance training, mechanical stress on muscle fibers is a key signal for the body to initiate the repair and growth process. This stress leads to the release of specific prostaglandins, such as prostaglandin F2α (PGF2α). This particular prostaglandin is a powerful signaling molecule that:
Promotes Muscle Protein Synthesis: PGF2α helps to turn on the cellular machinery responsible for building new muscle tissue. It plays a role in activating key pathways involved in protein synthesis, leading to muscle hypertrophy.
Activates Satellite Cells: PGF2α is essential for the activation and proliferation of satellite cells. These are a type of stem cell that resides on the outside of muscle fibers. When muscle is damaged, satellite cells are activated and fuse with the existing muscle fiber, contributing their nuclei and helping to repair and build new muscle tissue.
This is where the potential conflict with aspirin arises. While aspirin is excellent at preventing dangerous blood clots, its mechanism of action—inhibiting prostaglandin production—can also interfere with the beneficial prostaglandins that are essential for muscle growth and repair. For this reason, some athletes and bodybuilders choose to avoid or limit the use of nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin after a heavy workout, preferring to allow the natural inflammatory and signaling processes to occur to maximize their gains.
The use of an analgesic like acetaminophen (Tylenol), which does not have the same powerful anti-prostaglandin effects as aspirin, is often preferred by athletes who need pain relief without potentially hindering muscle growth.