The Journey from Precursor to Hormone
Insulin doesn't just appear fully formed; it undergoes an intricate, multi-step creation process.
-
Preproinsulin: The Blueprint: Insulin is initially synthesized as a precursor molecule called preproinsulin.
-
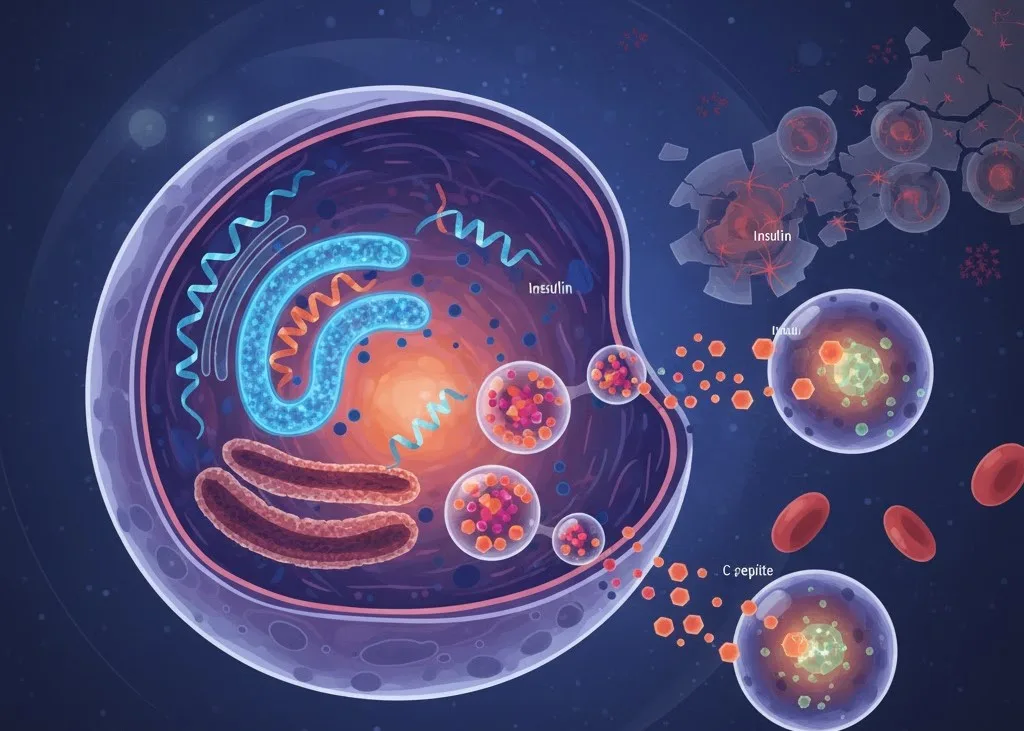
Proinsulin: The Intermediate: The preproinsulin is rapidly processed into proinsulin. This molecule acts as a single-chain structure where the future A-chain and B-chain of insulin are linked by a segment known as the C-peptide (connecting peptide). This C-peptide is crucial because it facilitates the correct folding of the proinsulin molecule, ensuring the active insulin hormone forms its proper structure.
-
Conversion and Storage: Inside the beta-cell's secretory granules, the proinsulin is cleaved, yielding two products in equal (equimolar) amounts: the mature, active insulin hormone and the biologically inactive C-peptide. Both are then stored in these granules, awaiting a signal for release.
As the abstract fragment notes: "Proinsulin is then converted to insulin and C-peptide and stored in secretory granules awaiting release on demand. Insulin synthesis is regulated at both the transcriptional and translational level." This highlights that the overall production rate of the hormone can be adjusted at the genetic level to meet the body's changing metabolic needs.
The Dynamics of Insulin Secretion
The main signal that triggers insulin release is an increase in blood glucose.
When blood glucose levels rise after a meal, the beta-cells take up the glucose and metabolize it. This process generates an intracellular signal (primarily an increase in ATP, followed by an influx of calcium ions) that acts as the "release on demand" mechanism, causing the secretory granules to fuse with the cell membrane and spill their contents—insulin and C-peptide—into the bloodstream.
Other nutrients like free fatty acids and amino acids, as well as various hormones (like GLP-1 and melatonin), can also fine-tune and amplify this glucose-induced secretion.
Beta-Cell Dysfunction: The Path to Diabetes
The core focus of this research article lies in the failure of this system, known as beta-cell dysfunction.
In both Type 1 and Type 2 diabetes, the beta-cells can't keep up with the body's demands.
-
Type 1 Diabetes: This is typically an autoimmune disease where the immune system mistakenly destroys the insulin-producing beta-cells, leading to an absolute lack of insulin.
-
Type 2 Diabetes: This is more complex, beginning with insulin resistance (where the body's cells don't respond well to insulin). The beta-cells initially try to compensate by overworking and releasing more insulin. Over time, however, they become exhausted and lose the ability to produce or secrete enough insulin, leading to eventual failure.
The article explores how genetic and environmental factors (such as chronic hyperglycemia, dyslipidemia, and inflammation) stress the beta-cells, eventually leading to their dysfunction and the development of the disease.
Understanding the precise molecular controls over insulin synthesis and secretion is vital because it helps researchers identify new targets for therapies that can protect, restore, or regenerate these crucial pancreatic beta-cells.