It's a common misconception to immediately label any discomfort or redness after an injection as an abscess. While a true abscess is a serious complication requiring medical attention, the initial pain and mild inflammation are often a normal inflammatory response to the injection itself. Understanding the timeline and symptoms is crucial to differentiate between a typical reaction and a developing infection.
The Initial Hurt: Your Body's Immediate Response
That initial sting and subsequent soreness you feel right after an injection are primarily due to the physical act of the needle piercing the skin and muscle tissue, as well as the injected substance itself causing localized irritation. Your body's natural inflammatory response kicks in immediately.
This normal inflammatory response can manifest as:
-Localized pain or tenderness at the injection site.
-Mild warmth.
-Slight redness.
These symptoms typically appear within the first few hours after the injection and are often most noticeable on the first day.
The Danger Signs: When to Suspect an Infection or Abscess
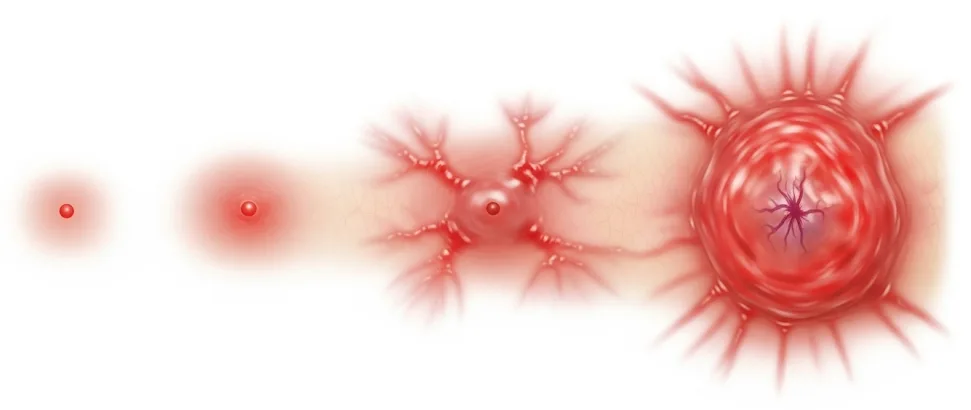
It is incorrect to assume that pain immediately after an injection signifies an abscess. A true infection and potential abscess usually take time to develop. If you experience a combination of worsening symptoms 3-4 days after the injection, it could indicate a developing infection and possible abscess formation.
Signs and symptoms that warrant concern and medical attention include:
Increasing pain: The pain becomes more severe and throbbing, rather than gradually subsiding.
Significant warmth: The injection site becomes markedly hot to the touch.
Fever: An elevated body temperature.
Headache: Especially if accompanied by other signs of illness.
spreading redness: The redness around the injection site expands significantly.
Noticeable inflammation: Swelling that increases over time.
General weakness or malaise: Feeling unwell overall.
Possible pus drainage: If an abscess has formed, you might see or feel a collection of fluid (pus) under the skin.
It's crucial to understand that these signs generally do not appear within the first 24 hours after a standard injection. The initial soreness is usually an inflammatory response, not an active infection.
Prevention is Key: Sterility Matters
The most critical step in preventing injection site infections and abscesses is maintaining strict sterility during the injection process. This includes:
Sterilizing the injection site: Thoroughly cleanse the skin with an antiseptic wipe (like alcohol) before injecting.
Using sterile needles and syringes: Never reuse needles or syringes.
Managing Initial Injection Site Discomfort
If you experience the typical soreness and mild inflammation in the first 8-24 hours after an injection, here's a step-by-step approach you can consider:
1. Warm Compress (First 8-12 Hours):
If you know you are prone to injection site discomfort or are injecting a potentially irritating substance, applying a warm compress during the first 8-12 hours might help to increase blood flow to the area. This could potentially aid in the dispersal of the injected substance and reduce initial localized irritation. However, this is most useful in the very initial hours.
2. Cold Compress (After 12-24 Hours):
Once the initial warmth subsides (typically after 12-24 hours), and if you are experiencing continued pain and inflammation, switch to a cold compress. Applying cold can help to constrict blood vessels, reduce swelling, and alleviate pain associated with the inflammatory response.
3. Local Topical NSAIDs (If Compress Doesn't Help):
If the pain and inflammation persist despite warm and cold compresses, consider using a local nonsteroidal anti-inflammatory drug (NSAID) cream or gel, such as piroxicam. Apply it to the affected area as directed on the product label, usually two to three times a day.
4. Oral NSAIDs (If Topical Doesn't Help):
If local NSAIDs are insufficient in managing your discomfort, you can consider taking oral NSAIDs. Common and often effective options include:
-Ibuprofen (e.g., Brufen, Advil)
-Naproxen (e.g., Naprosyn, Aleve)
-Nabumetone
-Combination products like Gelophen (which often contains ibuprofen and sometimes other analgesics)
Follow the recommended dosage on the packaging or as advised by a healthcare professional. Ibuprofen and Naproxen are often considered particularly useful for managing muscle and inflammatory pain.
5. Injectable NSAIDs (If Oral NSAIDs Don't Help and Pain is Severe):
If oral NSAIDs are not providing adequate relief and the pain is significant, especially if you suspect a severe inflammatory reaction (but without signs of infection), a healthcare professional might consider a local injection of an NSAID, such as ketorolac, into the affected area. This should only be done by a qualified medical practitioner.
Important Considerations:
Allergies: If you know you are allergic to a particular injected substance, applying a warm compress in the initial hours might help the substance disperse more quickly, potentially reducing the risk of a severe localized reaction.
Progression of Symptoms: It's crucial to continuously monitor your symptoms. If, at any point, you develop the warning signs of infection (increasing pain, significant warmth, spreading redness, fever, headache, weakness), seek immediate medical attention. Do not rely solely on home remedies.
Surgery for Abscess: If an abscess (a localized collection of pus due to infection) develops, it typically requires surgical drainage by a healthcare professional. Antibiotics are also usually necessary to clear the infection.